Cardiovascular Risk Factors
by Duane Graveline, MD, MPH
If a person has a strongly positive family history with a parent, a sibling, or aunts and uncles having died prematurely of heart attack or stroke, this person is at high risk even though no special testing is done.
Or if this individual has ECG changes of a silent myocardial infarction or clinical evidence of stroke warnings, high risk can be assumed.
So a positive family or personal history is perhaps the most definitive evidence of risk making irrelevant any normal test results in the blood test battery. Additionally, smoking, inactivity, hypertension, diabetes and excessive alcohol consumption are all silent partners in cardiovascular risk elevation.
Once they have obtained this information, most doctors would order blood tests. There are four that must be considered as highly relevant: the C-reactive protein, homocysteine, fibrinogen and lipoprotein(a) tests.
To be a good screening test it is important that means are available to correct the test results if they are abnormal. Lack of agreement on the various means for fibrinogen reduction weakens fibrinogen screening somewhat.
C-reactive protein:
C-reactive protein (CRP) is a protein found in the blood that is associated with the presence of inflammation somewhere in the body. It binds to chemicals on the surface of dead and dying cells in order to activate the complement system.
CRP was originally discovered in 1930 as a substance in the serum of patients with acute inflammation. Known as an acute phase reactant, it is believed to play an important role in innate immunity, as an early defense system against infections.
CRP rises up to 50,000-fold in acute inflammation, such as infection. It rises above normal limits within 6 hours, and peaks at 48 hours.
The high-sensitivity CRP (hs-CRP) test measures low levels of CRP using laser technology. The test gives results in 25 minutes with a special sensitivity for low values. Normal concentration in healthy human serum is usually lower than 10 mg/L,
Arterial damage results from white blood cells and inflammation within the wall. CRP can be thought of as a general marker for inflammation and infection, so it is now being used as a screening test for heart disease risk.
CRP is not a very specific test. Nevertheless, a level slightly above 2 mg/l has been associated with a doubling of the risk of a coronary event (plaque or blockage) compared to levels below 1 mg/l. The implications for mass screening with this test are profound compared with cholesterol which appears to be irrelevant to the atherosclerosis process.
Lipoprotein (a):
Lipoprotein(a) is also known as Lp(a) and is generally accepted as a useful predictor of cardiovascular risk. It was discovered in 1963.
High Lp(a) in blood is a risk factor for cerebrovascular disease, cardiovascular disease and atherosclerosis. Diet, exercise, and other environmental factors have little effect on Lp(a) concentrations although alcohol has been shown in numerous studies to have a lowering effect. Statins or other cholesterol lowering drugs have no effect on Lp(a).
Linus Pauling suggested that the gene responsible for this highly thrombogenic substance appears to have originated as far back as 45 million years ago. It is interesting to suppose the benefit of this strongly thrombogenic substance came at a time when man was emerging from an arboreal to terrestrial existence with greater exposure to tooth and claw.
It is appealing to think there might be great advantages for more rapid clotting of blood then. Today, there is no evidence that plasma Lp(a) is vital with persons having low Lp(a) appearing healthy. The reason for this gene could well be the hostile environment of the past.
Lp(a) concentrations vary widely among individuals (from < 0.2 to > 200 mg/dL), a range which is observed in all populations studied. Additionally there are distinct peculiarities in Lp(a) levels between different world populations with levels being two to three-fold higher in populations of African descent compared to Asian, Pacific, or European populations.
Because of the higher coagulant risk of lipoprotein(a), those with high values would benefit from reduction of these levels. Niacin and aspirin are two relatively safe, easily available and inexpensive drugs known to reduce the levels of Lp(a) in some individuals.
Note that the "conventional" risk threshold of 30 mg/dl would classify up to 50% of the individuals in some African populations as being at risk. Furthermore, Lp(a) measurement is in urgent need of standardization.
Homocysteine:
Homocysteine as a marker of cardiovascular disease risk has been very adequately described in the book, The Homocysteine Revolution by Kilmer McCully. I will add a few more observations appearing since his book on this subject was published.
There is now general agreement of the important role of homocysteine in atherosclerosis prevention. Earlier studies had demonstrated that lowering homocysteine cannot by itself reverse established pathology, its role appears to be more one of prevention.
Reducing homocysteine does not quickly repair existing structural damage of the artery. However, as McCully points out, the science is strongly supporting the biochemistry that homocysteine degrades and inhibits the formation of the three main structural components of the artery, collagen, elastin and the proteoglycans.
Simply put, homocysteine is a 'corrosive' of long-living proteins, i.e. collagen or elastin, or life-long proteins, i.e. fibrillin. These long-term effects are difficult to establish in clinical trials focusing on groups with existing artery decline.
A high level of blood serum homocysteine, "homocysteinemia" is a powerful risk factor for cardiovascular disease. This importance has now crossed over to the skeletal system.
Of note in addition to the cardiovascular risk is the observation that elevated levels of homocysteine have been linked to increased fractures in elderly persons. Homocysteine does not affect bone density. Instead, it appears that homocysteine affects collagen by interfering with the cross-linking between the collagen fibers and the tissues they reinforce.
Vitamins B6, B12 and folic acid remain the primary means for reducing homocysteine elevation. Each of these vitamins plays a role in the metabolism of homocysteine. Any one of these vitamins when deficient, may cause homocysteine elevation or any combination of these three vitamins may be involved Some people are born with a deficiency in all three of these vitamins, predisposing them to premature heart disease and stroke unless it is identified early on the basis of homocysteine elevation.
Fibrinogen:
Fibrinogen testing is usually ordered with other blood clotting tests. It helps your doctor to evaluate your body's ability to form a blood clot or in screening for increased cardiovascular disease risk.
Fibrinogen may be ordered as a follow-up to an abnormal prothrombin time or partial thromboplastin time — so well-known to those having to take a blood thinner — or for anyone experiencing an episode of prolonged or unexplained bleeding. It may be measured, along with tests such as PT, PTT and platelets for other serious bleeding or even clotting conditions.
Sometimes fibrinogen is ordered, along with other cardiac risk markers such as C-reactive protein, to help determine a patient's overall risk of developing cardiovascular disease.
This use of fibrinogen has not gained widespread acceptance though because there are no direct treatments for elevated levels. However, many doctors feel that fibrinogen measurements give them additional information and are well worth the time and expense.
Fibrin helps blood platelets to make a stable clot, more effectively sealing the leak in the circulatory system. Normal fibrinogen levels usually reflect normal blood clotting ability. Fibrinogen is an acute phase reactant — meaning that fibrinogen concentrations may rise sharply in any condition that causes inflammation or tissue damage.
Elevated concentrations of fibrinogen are not specific — they do not tell the doctor the cause or location of the disturbance. Elevated levels may be seen with coronary heart disease and myocardial infarction, but other contributors like autoimmune disease and acute infections have to be ruled out first.
You will notice that cholesterol is not on this list of screening tests for increased cardiovascular risk. This is because cholesterol appears increasingly irrelevant to arterial vascular disease and atherosclerosis.
Transfat consumption, smoking, hypertension and silent infections are among the triggers associated with the initial endothelial damage that starts the atherosclerotic process.
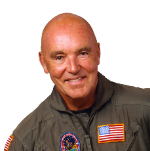
Duane Graveline MD MPH
Former USAF Flight Surgeon
Former NASA Astronaut
Retired Family Doctor
Updated June 2016